Unsurpassed Patient Experience.
Read their stories.






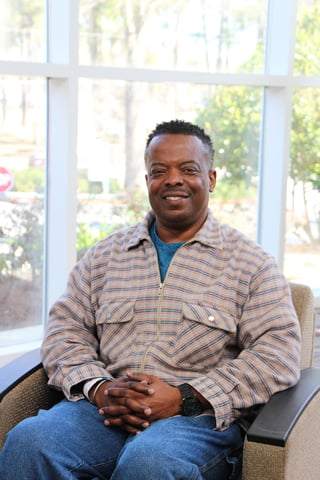
Marvin Edwards.
Cancer.
In the midst of the coronavirus pandemic, Marvin Edwards, 54, was diagnosed with colon cancer. With his primary doctor located in Tallahassee, Edwards began radiation treatments at a local healthcare facility.
It didn’t take long for the 140- mile roundtrip drive to become overwhelming. “The appointments were sometimes twice a week, and it was getting difficult to manage the treatments and work.”
Edwards, who is self-employed, started looking at other options. “It didn’t dawn on me until I started driving back and forth that maybe I should check with the hospital in Valdosta,” he said.
After a few inquiries, Edwards started radiation treatments at South Georgia Medical Center’s Pearlman Cancer Center. Accredited by the American College of Surgeons Commission on Cancer, the Pearlman Cancer Center team of fellowship-trained pathologists, surgeons, hematologists/medical oncologists, and radiation oncologists provide full-service clinics and advanced treatments.
Because cancer treatment requires a complex blend of medical and emotional care, each patient is assigned a nurse navigator to walk them through the process.
From his first day of treatment at Pearlman, Edwards said he was warmly welcomed and personally guided through the treatment process.
Under the medical care of Dr. Samuel Ofori, Edwards said, “Before I get to the next step in my treatments, Dr. Ofori is already getting things ready.”
Pleased that he transferred to SGMC, Edwards said he feels like a part of the Pearlman Cancer Center family.
“When you have cancer, you hear a lot of different things about what can happen, and you really don’t know what to expect,” Edwards said. “Dr. Ofori is leading me in the right direction, and that gives me a lot of peace.
“I wasn’t expecting this type of personal attention,” he said. “Here, they keep you informed every step of the way. If I need paperwork completed, I know Ms. Tamara [Lane] is going to take care of it. I don’t have to worry.”
Subscribe for updates Read more patient stories.

Ed Yarbrough.
Cardiology.
Big Thanks to Dasher Memorial Heart Center
Ed Yarbrough, 59, has always been physically active and dedicated to his workout routine that includes running, high-intensity CrossFit training, and Brazilian jiu-jitsu.
In August 2020, Yarbrough, an officer with the Nashville Police Department, decided to increase his exercise routine. “For about a week, I was on this big physical fitness kick,” he said. “I was feeling great. Then on Thursday, I spent all day working in my yard. It was one of those really hot days; it felt like 110 degrees. I overdid it and felt like I was dehydrated and went to the emergency room.”
With symptoms including dizziness, weakness, and tingling sensation in his chest, Yarbrough was admitted to South Georgia Medical Center, where Dr. Robert Collins, a Cardiologist, performed a series of tests.
“Dr. Collins was concerned that my troponin levels were high,” Yarbrough said. “He performed an echo [echocardiogram], and it came back normal. I was discharged and told his office would schedule an outpatient stress test.”
During his follow-up appointment, Yarbrough completed a treadmill stress test, which included an electrocardiogram (EKG).
“I got on the treadmill and felt fine,” he recalled. “They kept turning up the speed and still no problem. I felt fine, no problems.”
Yarbrough said he was “shocked” when he was told he needed to go immediately to SGMC’s catheterization laboratory (cath lab) for more tests.
After the heart catheterization, Yarbrough was informed by Dr. George S. Staton, a Cardiologist, that he needed open-heart surgery. “It all happened so quickly,” he recalled. “I didn’t have any chest pains. I don’t have high blood pressure, and I don’t smoke or drink. Having heart problems was not on my list.”
Yarbrough’s wife, Felicia, said, “We had no idea Ed was going to have issues with his heart and thought he would just have a stress test and go home.”
Once admitted to SGMC’s Cardiac Intensive Care Unit (CICU), located in the Dasher Memorial Heart Center, Dr. Joe Johnson, a Cardiothoracic Surgeon, was scheduled to perform Yarbrough’s open-heart surgery.
“Dr. Johnson came in and explained what would happen during the surgery,” he said. “I still was very anxious and had a lot of thoughts going through my mind.”
Felicia Yarbrough, a manager for SGMC’s Case Management and Transfer Center, recalled how one of the CICU nurses sensed her husband’s apprehension. “She asked one of the other patients, who was recovering from the same surgery, to speak with him. When my husband saw how well the patient was doing after the surgery, it immediately put his mind at ease. All the nurses were exceptional on the floor. They were attentive, caring, and compassionate.”
Yarbrough echoed his wife’s praise about the CICU team. “I’m not an emotional guy, but I will tell you that they are the most caring group of people. I received the best care possible at SGMC.”
Months after open-heart surgery, Yarbrough is working toward returning to his pre-surgery exercise routine and said, “I can tell you the entire third-floor staff at the Dasher Heart Center is amazing.”

Larissa Baker: The Gift of Life.
Labor & Delivery.
Two weeks before participating in a half-marathon, Larissa Baker, 32, found out she was expecting her third child.
“It was definitely a surprise pregnancy,” Larissa said. “I had been training for the half-marathon and thought my extreme hunger was from all the running.”
Larissa and her husband, Michael, were busy parents with two toddlers, RaeLyn and Charlotte, when they found out she was 11 weeks pregnant.
“The pregnancy was overall easy, much like my other two,” Larissa said. “I kept running and doing strength training until about 36 weeks, then started walking and strength training five to six days a week.”
After her due date had come and gone, Larissa’s nurse midwife, Teresa Johnson, scheduled her to be induced on September 14, 2020, at The Birthplace, located at South Georgia Medical Center.
“When I arrived at SGMC, I was dilated two centimeters, and everything was going good,” she said. “Later, when it was time for me to start pushing is when things started to go bad.”
At this point, she went into respiratory arrest, and SGMC’s emergency code team was immediately activated.
“She arrested and stopped breathing,” said Dr. Roy Swindle, an Obstetrician with Southern OB/GYN. “When they called a ‘code,’ all the emergency personnel showed up, and I was there within minutes. The nurse midwife, nurses, and anesthetist were all there. In a very short period, the decision was made to do an emergency C-section.”
Swindle explained that she developed an amniotic fluid embolism, a life-threatening, acute, and unexpected complication that can occur during delivery and affect both mother and baby.
A rare condition, Swindle said, amniotic fluid embolism occurs in approximately one in every 20,000 deliveries, and about 50 percent of women die within an hour of it happening.
“Some of the amniotic fluid got into her bloodstream and went to her lungs,” Swindle said. “Then she went into a condition called disseminated intravascular coagulopathy. She was using all her clotting factors and at a high risk of bleeding to death both internally and externally.”
“Everyone was where they were supposed to be to save my wife and son’s life,” Michael said. “They kept me very informed throughout the entire process even though I was in shock for most of it.”
After being stabilized, Larissa was moved to SGMC’s Intensive Care Unit (ICU). Her son, Rhett, born weighing 8 pounds, was immediately transported to the Neonatal Intensive Care Unit (NICU) at Phoebe Putney Memorial Hospital in Albany, Georgia.
While SGMC’s emergency response team cared for Larissa and her baby, Cathy Swilley, a nurse manager with Women’s and Children Services, checked on Michael.
“When they took me back for the C-section, Michael saw me have a seizure, and Cathy came and sat with him,” Larissa said. “She knew we didn’t have family here.”
After spending six days in ICU, Larissa was moved to a postpartum room. “All of this time, Rhett was still in Albany,” she said. “My parents came from Texas, so they could be with him during the day, while Michael stayed with me.”
On September 22, mother and son were united. “It had been a week, and I still hadn’t met my son,” she said. “My parents would send pictures, but it was difficult not being with him. They brought him to SGMC, and shortly afterward, I was discharged, and we both went home.”
Larissa appreciates the kindness and attention she and Michael received. “They were all great,” she said. “They helped get Michael a place to stay at the hospital. When I was in ICU, he could stay during the day, and then at night had a room at the hospital to sleep.”
Michael said having the room at SGMC was extremely helpful. “I told the staff I would not be leaving the hospital until my wife did. I was prepared to sleep in my truck if I had to. The room was awesome, and the nurses spoiled me with a big bag of snacks to get me through.
“Dr. Swindle called to debrief me most nights to keep me updated on Larissa’s condition. Our midwife, Teresa Johnson, did the same in the afternoons,” he said. “Two of the greatest human beings I’ve ever met. We are extremely blessed that they were a part of all of this.”
Subscribe for updates Access more inspiring stories.

Raygen Youngblood.
Neurosurgery Improves Quality of Life.
An active 14-year-old, Raygen Youngblood has overcome numerous physical obstacles. She was born premature, weighing 1 pound, 10 ounces, and spent many weeks in a neonatal intensive care unit, where she experienced two Grade 4 strokes.
Raygen’s mom, Harriet Youngblood, explained, “There was so much blood leaking in her brain that it couldn’t be absorbed. It caused a large clot and tumor to form. When she had the second stroke, we were told she would be blind, deaf, and on a feeding tube. But God had a different plan.”
While struggling with generalized tonicclonic seizures, also called grand mal seizures, Raygen has been able to excel academically and is a member of the Southside Christian School cross country team and drama club.
“She has been through so much,” Harriet said. “Raygen has cerebral palsy and hemiplegia. Her right side is partially immobile because of the strokes.”
Examined by numerous neurologists, Harriet said the consensus is the tumor is inoperable, leaving Raygen dependent on daily medication and little hope for a seizure-free life.
Raygen’s despair finally gave way to hope when her neurologist Dr. Hernan Posas recommend a vagus nerve stimulator (VNS), a medical device designed to prevent seizures before they start and stop if they occur.
Posas referred Raygen to Dr. Kimberly Mackey, a neurosurgeon at South Georgia Medical Center. While the VNS procedure is not new, Mackey is the only board-certified pediatric neurosurgeon in South Georgia that performs VNS therapy.
Mackey, who has been performing VNS therapy for the past 11 years, explained that the device sends mild pulses through the vagus nerve to areas of the brain associated with seizures. People with a VNS often experience fewer seizures, and if seizures occur, they are usually shorter and less severe with better recovery.
The VNS is used in conjunction with medication or other treatments for people 4-years-old and older with drug-resistant epilepsy and focal (partial-onset) seizures.
Raygen also wears a magnet around her wrist. When she feels a seizure coming on, she can waive the magnet over her VNS.
“Having Dr. Mackey come to SGMC has been a blessing for our family,” Harriet said. “When we first went to meet her, she spoke directly to Raygen. She wanted to make sure Raygen wanted to go through with the surgery. It was up to her.”
For Raygen, the VNS represents a better quality of life. “Before, I wasn’t sure if I would ever be able to live on my own or even get a driver’s license,” said Raygen, who one day wants to be a forensic scientist.